Diabetes is a chronic metabolic disorder that affects millions of people worldwide, characterised by elevated blood glucose levels due to the body’s inability to produce or effectively use insulin. There are two main types of diabetes – type 1, where the body doesn’t produce insulin, and type 2, where the body becomes resistant to insulin or doesn’t produce enough.
Proper blood glucose monitoring is essential for reducing the risk of diabetes-related complications such as heart disease, kidney problems, and nerve damage.
The Importance of Blood Glucose Management
Keeping your blood glucose levels within target ranges is essential for preventing both short-term and long-term complications. Your healthcare team will help you set personalised targets based on your individual needs.
Risks of Poor Diabetes Management
Failing to manage diabetes effectively can lead to serious health complications, including:
- Cardiovascular disease
- Kidney damage (nephropathy)
- Eye problems (retinopathy)
- Nerve damage (neuropathy)
- Foot problems
- Increased risk of infections
Lifestyle Changes for Diabetes Management
Healthy Eating
A balanced diet is crucial for managing diabetes. Focus on:
- Choosing complex carbohydrates over simple sugars
- Incorporating plenty of fruits, vegetables, and whole grains
- Limiting saturated fats and processed foods
- Controlling portion sizes
Regular Physical Activity
Exercise helps improve insulin sensitivity and manage blood glucose levels. Aim for:
- At least 150 minutes of moderate-intensity aerobic activity per week
- Strength training exercises 2-3 times per week
- Incorporating movement into your daily routine
Maintaining a Healthy Weight
If you’re overweight, losing even a small amount of weight can significantly improve blood glucose control. Work with your healthcare team to set realistic weight loss goals.
Stress Management
Stress can affect blood glucose levels. Try incorporating stress-reduction techniques such as:
- Mindfulness meditation
- Deep breathing exercises
- Yoga or tai chi
Limiting Alcohol and Quitting Smoking
Excessive alcohol consumption can interfere with diabetes management. If you choose to drink, do so in moderation. Smoking increases the risk of diabetes complications, so quitting is strongly recommended.
Medication and Monitoring
Taking Prescribed Medications
Depending on your type of diabetes and individual needs, your healthcare team may prescribe:
- Insulin injections or pumps
- Oral medications (e.g., metformin)
- Other injectable medications
It’s crucial to take medications as prescribed and discuss any concerns with your healthcare provider.
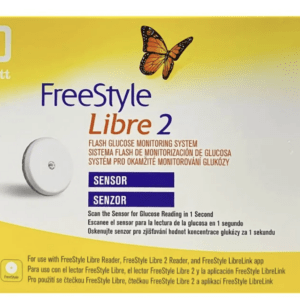
Regular Blood Glucose Monitoring
Self-monitoring of blood glucose levels helps you understand how food, activity, and medication affect your diabetes. Your healthcare team will advise on how often to check and what your target ranges should be.
HbA1c Testing
This blood test measures your average blood glucose levels over the past 2-3 months. Aim to have this test at least twice a year.
Regular Check-ups and Screenings
Attend all scheduled appointments with your diabetes care team. Regular check-ups typically include:
- Blood pressure measurements
- Foot examinations
- Eye screenings
- Kidney function tests
- Cholesterol level checks
Diabetes Education and Support
Staying informed about diabetes management is crucial. Consider:
- Attending diabetes education programmes
- Joining support groups or online communities
- Using reliable resources like Diabetes UK for up-to-date information